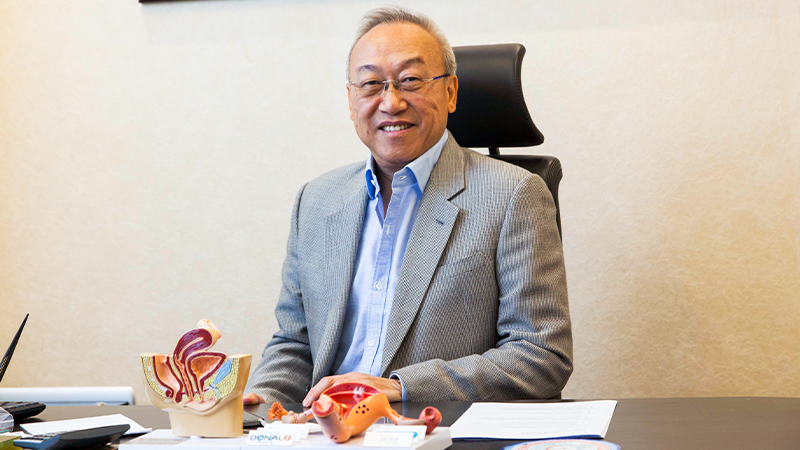
Miscarriage is something that few people are willing to talk about – yet as many as 23 million miscarriages occur worldwide each year. It’s an important discussion to have, too, not only for the support that it can provide for grieving parents, but also because it shines a spotlight on the treatments available. This is especially true for those who have experienced what’s known as recurrent miscarriage (an estimated one to three percent of couples and 10 percent of pregnancies). Professor MILTON LEONG, Specialist in Reproductive Medicine in Hong Kong, addresses some key questions about miscarriages – risk factors, causes and reasons why IVF treatment might be needed.
How do we define recurrent miscarriage?
For most couples who have no reason to fail, 80 percent or so will successfully get pregnant within 12 months. However, within the first two to three months, 15 to 20 percent of these early pregnancies may not progress medically. Those are miscarriages. If there are three consecutive miscarriages, then it is said to be recurrent. For those who went through assisted reproduction, the miscarriages may even show up as failures.
The good news is that recurrent miscarriages and failure of implantation may be treatable, so their cases need to be investigated.
To what extent is age a factor in early miscarriage?
Maternal age is a known risk factor of miscarriage, largely because chromosomal abnormalities in the foetus happen more frequently when a woman gets older. The chance of miscarriage is 10 to 15 percent for women below 30 years old, but may be 30 percent at age 35, and more than 50 percent for women over age 40.
The main causes of this are twofold: firstly, because the “eggs” are getting “old” with age and genetically or functionally changed; and secondly, because the embryos made are abnormal (40 percent at age 35, up to 80 percent at 40 and above).
What can we do about miscarriages?
Largely, early miscarriages may be just bad luck – reasons can include an abnormal embryo or an unfavourable hormonal environment at the time. But when a single miscarriage becomes a series of miscarriages, it warrants investigation and seeking a diagnosis.
At this point, it’s better to consult a doctor experienced in the field; then, if any cause does come to light, appropriate treatment can be planned.
For example, uterine structural abnormalities can be treated with surgery, while medical treatment can improve hormonal deficiency and modulate the immune response. Some genetic diseases can be dealt with using preimplantation genetic tests (PGT) to select the normal embryos. Early assessment will help you to identify causes of conception difficulty.
5 main causes of a first trimester miscarriage
#1 Genetic abnormalities
More than half of all first trimester miscarriages are the result of the baby having abnormal chromosomes. If your body detects that the foetus has damaged or missing chromosomes, it will end the pregnancy. In rare cases, one or both of the parents may themselves have a genetic defect, which would impact on the foetus they produce (for example, Robertsonian translocation, or ROB).
#2 Autoimmune disorder
Growing a baby inside the uterus requires adaptations much like any other organ transplantation. Sometimes this “tolerance” is absent, and the embryo or the developing foetus may be “rejected”. Much of this is still not clearly known, but experience has shown that certain factors can be tested and if they’re found to be “rejecting” a foetus, they can be altered to promote tolerance; this, in turn, can reverse or prevent the rejection process, leading to successful live births.
#3 Placental problems
The placenta is an organ that grows in the womb during pregnancy, and if the foetus and placenta are not compatible, the pregnancy may be lost. Likewise, uterine defects, including an abnormal shape, tumours like fibroids and adenomyosis, and adhesions in the uterine cavity, may also cause the sudden ending of a pregnancy.
#4 Hormonal imbalance
Imbalance of certain hormones, for example progesterone, prolactin or thyroid hormone, can result in miscarriage. Progesterone is especially important because it helps to maintain the endometrium lining; if there are low levels of progesterone, the lining may not be ready to support the pregnancy.
#5 Ectopic pregnancy
This potentially serious but rare type of pregnancy occurs when the foetus begins developing outside the womb. Ectopic pregnancies cannot be saved and are a medical emergency requiring immediate treatment.
Five reasons why IVF treatment may be needed
#1 Poor sperm or low sperm count
#2 Ovulation problems, including age-related issues
#3 Blocked or damaged fallopian tubes
#4 Ovarian conditions including endometriosis or polycystic ovary syndrome (PCOS)
#5 Unexplained reasons
Dr Leong advises consulting and choosing a gynaecologist sooner rather than later so you can shorten the interval between planning and a successful birth. Read more stories on women’s health at expatliving.hk/health-fitness.
Watch the video below to see more about the IVF treatment process.
This article first appeared in the Autumn 2022 issue of Expat Living magazine. Subscribe now so you never miss an issue.







